現在位置 : RA > 認識 免疫調節藥 - Hydroxychloroquine (HCQ) - Plaquenil
|
認識 免疫調節藥 - Hydroxychloroquine (Plaquenil, 必賴克婁,俗稱奎寧或瘧疾藥)
一種常用的風濕病用藥,副作用包括腸胃不適,皮疹或皮膚黑,癢,視網膜病變(停藥可慢慢恢復),但是長期使用尚稱安全,長期使用時醫師會定期抽血追蹤。 適應症 -- Treatment of Acute attacks of malaria;discoid and systemic lupus erythematosus and rheumatoid arthritis. 風濕性關節炎、慢性多形性日光疹、慢性圓板狀紅斑症、瘧疾。 常見副作用 -- Agranulocytosis, leukopenia,aplastic anemia, ataxia, seizures, vertigo, visual disturbance,anorexia, nausea, vomiting, diarrhea, pruritis, weight loss , bleaching of hair. 禁忌(症) -- Patients with retinal or visual field change; hypersensitivity; long-term therapy in children. 常用劑量及頻次 -- RA Adult Initially 400-600 mg daily. Maintenance: 200-400 mg daily. Juvenile chronic arthritis 6.5 mg/kg body wt/day or 400 mg/day, whichever is smaller. Systemic or discoid lupus erythematosus Adult Initially 400-800 mg daily. Maintenance: 200-400 mg daily. 注意事項與警語 -- Use cautiously in patients with severe GI, neurologic blood disorder; and patients with hepatic disease, or alcoholism, G6PD deficiency. During long-term therapy, blood cell count and liver function studies should be made. 視力模糊或任何其他眼毒性 1. 請勿自行停藥 2. 若症狀未見改善,請與醫師連絡 |
|
Plaquenil(必賴克瘻)用藥教育
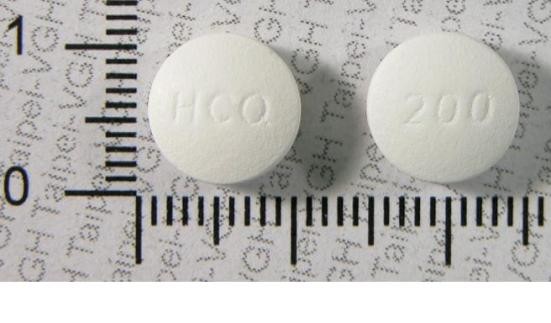
中壢天晟醫院 風濕免疫科 翁國益醫師 什麼是Plaquenil (必賴克瘻)? Plaquenil (必賴克瘻),學名是Hydroxychloroquine,是一種風濕免疫科醫師常用的疾病進程修飾性抗風濕藥物,用來治療各種發炎性關節炎及自體免疫疾病,如類風濕性關節炎、紅斑性狼瘡或乾燥症等等。Plaquenil (必賴克瘻)用在治療發炎性關節炎時,除了可以減輕關節的疼痛和腫脹之外,還可以減少關節被破壞,造成永久性殘障的機率。Plaquenil (必賴克瘻)也是一種抗瘧疾藥物,一開始是被使用在瘧疾的預防和治療上。Plaquenil (必賴克瘻)跟目前仍用在治療瘧疾的奎寧(quinine)是同一類,但並不相同的藥物。 Plaquenil(必賴克瘻)對身體有什麼作用?為什麼可以用來治療發炎性關節炎及自體免疫疾病? Plaquenil (必賴克瘻)作用在身體的免疫系統,是一種免疫調節劑。Plaquenil (必賴克瘻)會影響許多免疫細胞的功能及不同免疫細胞間的交互作用,所以可以治療許多發炎性關節炎及自體免疫疾病。 Plaquenil (必賴克瘻)怎麼服用?什麼時候才會產生療效? Plaquenil (必賴克瘻)一顆含有200公絲的有效成分,使用在風濕免疫科的適應症時通常須要每日服用400公絲,可以一次服用或分兩次服用。服用一段時間後醫師會根據臨床情況調整劑量。一般約在開始服用的四到八個星期後才會開始產生療效,最大的療效則可能在六個月後才會達到。 Plaquenil (必賴克瘻)有什麼副作用? Plaquenil (必賴克瘻)是一種非常安全,病患接受度非常高的藥物,嚴重的副作用非常少見。最常見的副作用是噁心或腹瀉,如果改為飯後服用大多都會改善。比較不常見的副作用有皮膚起疹子、輕微掉髮或髮色變淺及感覺虛弱無力。極罕見的副作用包括視力受影響,不過通常在高劑量、非常長期使用後才會發生,或是年紀大於六十歲,或是腎功能很差的病患。目前風濕免疫科醫師用Plaquenil (必賴克瘻)來治療發炎性關節炎及自體免疫疾病的劑量比以前用來治療瘧疾的劑量低很多,所以病患發生上述罕見副作用的情形比以前也更少見。 服用Plaquenil (必賴克瘻)的病患生活中有什麼應該特別注意的事? 雖然服用Plaquenil (必賴克瘻)引起視力受影響的機率很低,但是如果病患在服用Plaquenil (必賴克瘻)的過程中感覺視力有變化,當然還是要馬上跟醫師反應,安排進一步的眼科檢查。如果發現的早,在停止服用Plaquenil (必賴克瘻)之後視力大都可以恢復正常。希望懷孕和懷孕中的婦女需要和醫師討論是否服用Plaquenil (必賴克瘻),因為目前醫學上對於服用Plaquenil (必賴克瘻)會不會影響胚胎或受孕並沒有共識,醫師會針對每個病患不同的病情做最合理的建議。病患千萬不可以擅自停藥,如果因此造成病情惡化對於胚胎或受孕影響更大。原則上病患只要依照醫師處方正確服藥,了解可能發生的副作用,有任何不舒服立即與醫師聯絡,就可以放心接受Plaquenil (必賴克瘻)的治療。 (部分內容參考美國風濕學院網站) |
Hydroxychloroquine (Plaquenil) is an older DMARD sometimes still used for mild RA. It may work by interrupting signaling among cells. It’s one of the best tolerated DMARDs. Side effects are usually mild and may include nausea and diarrhea. Taking the drug with food may help. Changes to the skin are less common. These may include rashes or the appearance of dark spots. In extremely rare cases the drug may affect vision. Report any vision problems to your doctor immediately.
|
|
Hydroxychloroquine for Rheumatoid Arthritis
|
|
Hydroxychloroquine (HCQ)- Plaquenil
Hydroxychloroquine is an antimalarial drug, sold under the trade names Plaquenil, Axemal (in India), Dolquine and Quensyl, also used to reduce inflammation in the treatment of rheumatoid arthritis (see disease-modifying antirheumatic drugs) and lupus. Hydroxychloroquine differs from chloroquine by the presence of a hydroxyl group at the end of the side chain: The N-ethyl substituent is beta-hydroxylated. It is available for oral administration as hydroxychloroquine sulfate (plaquenil) of which 200 mg contains 155 mg base in chiral form. Hydroxychloroquine has similar pharmacokinetics to chloroquine, with quick gastrointestinal absorption and is eliminated by the kidney. Cytochrome P450 enzymes (CYP 2D6, 2C8, 3A4 and 3A5) N-desethylated Hydroxychloroquine to Ndesethylhydroxychloroquine. |
|
Medical Use
Hydroxychloroquine has been used for many years to treat malaria. It is also used to treat systemic lupus erythematosus, rheumatic disorders like rheumatoid arthritis and Sjögren's Syndrome, and porphyria cutanea tarda. Hydroxychloroquine increases[2] lysosomal pH in antigen presenting cells. In inflammatory conditions, it blocks toll-like receptors on plasmacytoid dendritic cells (PDCs)[citation needed]. Toll-like receptor 9 (TLR 9), which recognizes DNA-containing immune complexes, leads to the production of interferon and causes the dendritic cells to mature and present antigen to T cells. Hydroxychloroquine, by decreasing TLR signaling, reduces the activation of dendritic cells and the inflammatory process. Hydroxychloroquine is also widely used in the treatment of post-Lyme arthritis following Lyme disease. It may have both an anti-spirochaete activity and an anti-inflammatory activity, similar to the treatment of rheumatoid arthritis. Adverse effects The most common adverse effects are a mild nausea and occasional stomach cramps with mild diarrhea. The most serious adverse effects affect the eye. For short-term treatment of acute malaria, adverse effects can include abdominal cramps, diarrhea, heart problems, reduced appetite, headache, nausea and vomiting. For prolonged treatment of lupus or arthritis, adverse effects include the acute symptoms, plus altered eye pigmentation, acne, anemia, bleaching of hair, blisters in mouth and eyes, blood disorders, convulsions, significant vision difficulties, diminished reflexes, emotional changes, excessive coloring of the skin, hearing loss, hives, itching, liver problems or failure, loss of hair, muscle paralysis, weakness or atrophy, nightmares, psoriasis, reading difficulties, tinnitus, skin inflammation and scaling, skin rash, vertigo and weight loss. Hydroxychloroquine can worsen existing cases of both psoriasis and porphyria. Eyes One of the most serious side effects is a toxicity in the eye (generally with chronic use). The daily safe maximum dose for eye toxicity can be computed from one's height and weight using this calculator. Macular toxicity is related to the total cumulative dose rather than the daily dose. People taking 400 mg of hydroxychloroquine or less per day generally have a negligible risk of macular toxicity, whereas the risk begins to go up when a person takes the medication over 5 years or has a cumulative dose of more than 1000 grams. Regular eye screening, even in the absence of visual symptoms, is recommended to begin when either of these risk factors occurs. Toxicity from hydroxychloroquine may be seen in two distinct areas of the eye: the cornea and the macula. The cornea may become affected (relatively commonly) by an innocuous vortex keratopathy and is characterized by whorl-like corneal epithelial deposits. These changes bear no relationship to dosage and are usually reversible on cessation of hydroxychloroquine. The macular changes are potentially serious and are related to dosage and length of time taking hydroxychloroquine. Advanced retinopathy is characterized by reduction of visual acuity and a "bulls eye" macular lesion which is absent in early involvement. |
|
Overdose symptoms
Symptoms of overdose can occur within a half-hour of taking the medication. Overdose symptoms include convulsions, drowsiness, headache, heart problems or heart failure, difficulty breathing and vision problems. Mechanism of Action Antimalarials are lipophilic weak bases and easily go through plasma membranes. The free base form accumulates in lysosomes (acidic cytoplasmic vesicles) and is then protonated, resulting in concentrations within lysosomes up to 1000 times higher than in culture media. This increases the pH of the lysosome from 4 to 6. Alteration in pH causes inhibition of lysosomal acidic proteases causing a diminished proteolysis effect. Higher pH within lysosomes causes decreased intracellular processing, glycosylation, and secretion of proteins with many immunologic and nonimmunologic consequences. These effects are believed to be the cause of a decreased immune cell functioning such as chemotaxis, phagocytosis and superoxide production by neutrophils. HCQ is a weak diprotic base that can pass through the lipid cell membrane and preferentially concentrate in acidic cyto-plasmic vesicles. The higher pH of these vesicles in macrophages or other antigen-presenting cells limits the association of autoantigenic (any) peptides with class II MHC molecules in the compartment for peptide loading and/or the subsequent processing and transport of the peptide-MHC complex to the cell membrane. Recently a novel mechanism has been described wherein hydroxychloroquine inhibits stimulation of the toll-like receptor (TLR) 9 family receptors. TLRs are cellular receptors for microbial products that induce inflammatory responses through activation of the innate immune system. As with other quinoline antimalarial drugs, the mechanism of action of quinine has not been fully resolved. The most accepted model is based on hydrochloroquinine, this model involves the inhibition of hemozoin biocrystallization, which facilitates the aggregation of cytotoxic heme. Free cytotoxic heme accumulates in the parasites, causing their deaths. |
|
Hydroxychloroquine (HCQ) Side Effects
Some side effects of hydroxychloroquine may not be reported. Always consult your doctor or healthcare specialist for medical advice. You may also report side effects to the FDA. For the Consumer Applies to hydroxychloroquine: oral tablet Along with its needed effects, hydroxychloroquine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention. When this medicine is used for short periods of time, side effects usually are rare. However, when it is used for a long time and/or in high doses, side effects are more likely to occur and may be serious. Check with your doctor immediately if any of the following side effects occur while taking hydroxychloroquine: Less common • Blurred vision or any other change in vision—this side effect may also occur or get worse after you Stop taking hydroxychloroquine Rare • Convulsions (seizures) • increased muscle weakness • mood or other mental changes • ringing or buzzing in ears or any loss of hearing • sore throat and fever • unusual bleeding or bruising • unusual tiredness • weakness Symptoms of overdose • Drowsiness • headache • increased excitability Some side effects of hydroxychloroquine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them: More common • Diarrhea • difficulty in seeing to read • headache • itching (more common in black patients) • loss of appetite • nausea or vomiting • stomach cramps or pain Less common • Bleaching of hair or increased hair loss • blue-black discoloration of skin, fingernails, or inside of mouth • dizziness or lightheadedness • nervousness or restlessness • skin rash For Healthcare Professionals Applies to hydroxychloroquine: compounding powder, oral tablet General In general, although not every side effect listed in the side effects section may have been reported with the use of hydroxychloroquine, they have all been reported with the use of one or more 4-aminoquinoline compounds. Ocular Ocular side effects have included disturbances of accommodation with symptoms of blurred vision (dose-related and reversible with treatment cessation). Corneal side effects have included transient edema, punctate to lineal opacities, decreased corneal sensitivity, corneal changes (with or without accompanying symptoms, including blurred vision, halos around lights, photophobia), and corneal deposits. Retinal (macular) side effects have included edema, atrophy, abnormal pigmentation (mild pigment stippling to a "bullseye" appearance), loss of foveal reflex, increased macular recovery time following exposure to a bright light (photostress test), and elevated retinal threshold to red light in macular, paramacular, and peripheral retinal areas. Other fundus changes have included optic disc pallor and atrophy, attenuation of retinal arterioles, fine granular pigmentary disturbances in the peripheral retina, and prominent choroidal patterns in advanced stage. Visual field defects have included pericentral or paracentral scotoma, central scotoma with decreased visual acuity, rarely field constriction, and abnormal color vision. The most common visual symptoms attributed to retinopathy are reading and vision difficulties (words, letters, or parts of objects missing), photophobia, blurred distance vision, missing or blacked out areas in the central or peripheral visual field, and light flashes and streaks. Patients with retinal changes may have visual symptoms or may be asymptomatic (with or without visual field changes). Rarely scotomatous vision or field defects may occur without obvious retinal change. A few cases of retinal changes consisting of change in retinal pigmentation (detected on periodic ophthalmologic examination) with visual field defects in some instances have been reported in patients receiving only hydroxychloroquine. A case of delayed retinopathy with vision loss starting 1 year after hydroxychloroquine discontinuation has been reported. Night vision difficulties and immediate blurred vision have been reversible with treatment cessation. The corneal changes (fairly common) have been reversible. Corneal deposits have been reported as early as 3 weeks after the initiation of therapy. Retinopathy appears to be dose related and has occurred within several months (rarely) to several years of daily therapy. Gastrointestinal Gastrointestinal side effects have included diarrhea, anorexia, nausea, abdominal cramps, vomiting, and epigastric pain. A case of pigmentation of the gums has also been reported. Nervous system Nervous system side effects have included headache, dizziness, vertigo, tinnitus, nystagmus, nerve deafness, convulsions,and ataxia. Psychiatric Psychiatric side effects have included irritability, nervousness, emotional changes, nightmares, and psychosis. Musculoskeletal Musculoskeletal side effects have included skeletal muscle palsies, skeletal muscle myopathy, or neuromyopathy leading to progressive weakness and atrophy of proximal muscle groups which may be associated with mild sensory changes, depression of tendon reflexes, and abnormal nerve conduction. Absent or hypoactive deep tendon reflexes and extraocular muscle palsies have been reported. Neuromyotoxicity has been associated with hydroxychloroquine concurrently with worsening renal function. Dermatologic Mucocutaneous hyperpigmentation over all extremities, the torso, and the hairline has been reported in an elderly man after long-term hydroxychloroquine use. Skin biopsies demonstrated sharply defined red-brown fibers in the deep dermis and the classic "banana-shaped body" associated with exogenous ochronosis. Dermatologic side effects have included nonlight-sensitive psoriasis, bleaching of hair, alopecia, pruritus, skin and mucosal pigmentation, photosensitivity, and skin eruptions (urticarial, morbilliform, lichenoid, maculopapular, purpuric, erythema annulare centrifugum, Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, and exfoliative dermatitis). A case of generalized pustular drug rash has also been reported. Hematologic Hematologic side effects have included various blood dyscrasias such as aplastic anemia, agranulocytosis, leukopenia, anemia, and thrombocytopenia. Hemolysis has been reported in individuals with glucose-6-phosphate dehydrogenase deficiency. Cardiovascular The causal relationship of hydroxychloroquine to cardiomyopathy has not been established. Cardiovascular side effects have rarely included cardiomyopathy with high daily dosages. Hepatic Hepatic side effects have included isolated cases of abnormal liver function and fulminant hepatic failure. Metabolic Metabolic side effects have included weight loss and exacerbation or precipitation of porphyria. Other Other side effects have included lassitude. Hypersensitivity Hypersensitivity side effects have included allergic reactions (urticaria, angioedema, and bronchospasm) and hypersensitivity myocarditis. Endocrine Endocrine side effects have included a case report of hypoglycemia induced by hydroxychloroquine in a type II diabetic treated for polyarthritis. |
|
Plaquenil FDA Prescribing Information: Side Effects
(Adverse Reactions) SIDE EFFECTS MALARIA Following the administration in doses adequate for the treatment of an acute malarial attack, mild and transient headache, dizziness, and gastrointestinal complaints (diarrhea, anorexia, nausea, abdominal cramps and, on rare occasions, vomiting) may occur. Cardiomyopathy has been rarely reported with high daily dosages of hydroxychloroquine. LUPUS ERYTHEMATOSUS AND RHEUMATOID ARTHRITIS Not all of the following reactions have been observed with every 4-aminoquinoline compound during long-term therapy, but they have been reported with one or more and should be borne in mind when drugs of this class are administered. Adverse effects with different compounds vary in type and frequency. CNS Reactions: Irritability, nervousness, emotional changes, nightmares, psychosis, headache, dizziness, vertigo, tinnitus, nystagmus, nerve deafness, convulsions, ataxia. Neuromuscular Reactions: Skeletal muscle palsies or skeletal muscle myopathy or neuromyopathy leading to progressive weakness and atrophy of proximal muscle groups which may be associated with mild sensory changes, depression of tendon reflexes and abnormal nerve conduction. Ocular Reactions: A. Ciliary body: Disturbance of accommodation with symptoms of blurred vision. This reaction is dose-related and reversible with cessation of therapy. B. Cornea: Transient edema, punctate to lineal opacities, decreased corneal sensitivity. The corneal changes, with or without accompanying symptoms (blurred vision, halos around lights, photophobia), are fairly common, but reversible. Corneal deposits may appear as early as three weeks following initiation of therapy. The incidence of corneal changes and visual side effects appears to be considerably lower with hydroxychloroquine than with chloroquine. C. Retina: Macula: Edema, atrophy, abnormal pigmentation (mild pigment stippling to a "bull's-eye" appearance), loss of foveal reflex, increased macular recovery time following exposure to a bright light (photo-stress test), elevated retinal threshold to red light in macular, paramacular, and peripheral retinal areas. Other fundus changes include optic disc pallor and atrophy, attenuation of retinal arterioles, fine granular pigmentary disturbances in the peripheral retina and prominent choroidal patterns in advanced stage. D. Visual field defects: Pericentral or paracentral scotoma, central scotoma with decreased visual acuity, rarely field constriction, abnormal color vision. The most common visual symptoms attributed to the retinopathy are: reading and seeing difficulties (words, letters, or parts of objects missing), photophobia, blurred distance vision, missing or blacked out areas in the central or peripheral visual field, light flashes and streaks. Retinopathy appears to be dose related and has occurred within several months (rarely) to several years of daily therapy; a small number of cases have been reported several years after antimalarial drug therapy was discontinued. It has not been noted during prolonged use of weekly doses of the 4-aminoquinoline compounds for suppression of malaria. Patients with retinal changes may have visual symptoms or may be asymptomatic (with or without visual field changes). Rarely scotomatous vision or field defects may occur without obvious retinal change. Retinopathy may progress even after the drug is discontinued. In a number of patients, early retinopathy (macular pigmentation sometimes with central field defects) diminished or regressed completely after therapy was discontinued. Paracentral scotoma to red targets (sometimes called "premaculopathy") is indicative of early retinal dysfunction which is usually reversible with cessation of therapy. A small number of cases of retinal changes have been reported as occurring in patients who received only hydroxychloroquine. These usually consisted of alteration in retinal pigmentation which was detected on periodic ophthalmologic examination; visual field defects were also present in some instances. A case of delayed retinopathy has been reported with loss of vision starting one year after administration of hydroxychloroquine had been discontinued. Dermatologic Reactions: Bleaching of hair, alopecia, pruritus, skin and mucosal pigmentation, photosentivity, and skin eruptions (urticarial, morbilliform, lichenoid, maculopapular, purpuric, erythema annulare centrifugum, Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, and exfoliative dermatitis). Hematologic Reactions: Various blood dyscrasias such as aplastic anemia, agranulocytosis, leukopenia, anemia, thrombocytopenia (hemolysis in individuals with glucose-6-phosphate dehydrogenase (G-6-PD) deficiency). Gastrointestinal Reactions: Anorexia, nausea, vomiting, diarrhea, and abdominal cramps. Isolated cases of abnormal liver function and fulminant hepatic failure. Allergic reactions: Urticaria, angioedema and bronchospasm have been reported. Miscellaneous Reactions: Weight loss, lassitude, exacerbation or precipitation of porphyria and nonlight-sensitive psoriasis. Cardiomyopathy has been rarely reported with high daily dosages of hydroxychloroquine. DRUG INTERACTIONS No information provided. Read the entire FDA prescribing information for Plaquenil (Hydroxychloroquine) » |