現在位置 : 醫療 > 眼科 > 眼睛 白內障的治療 - Cataract Treatment
|
白內障 (Cataract)
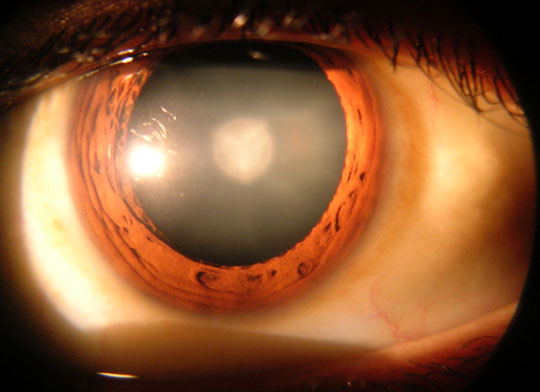
白內障疾病是首位致盲性眼病,白內障的流行情況各地區沒有差異,中醫中又稱「青盲」。一般來說,隨著年齡的增長,白內障的發病率逐漸提高。 晶狀體的混濁位置可以在皮質、核、前囊或者後囊等處。晶狀體的混濁不一定影響視力。出現在視軸上的混濁對視力的影響較大,例如後囊下的混濁,由於其處於眼球這個光學系統的節點處,所以即使是較小的混濁也對視力有較大的影響。 典型的白內障的臨床表現是漸進性視力下降,由於晶狀體的密度變化,還可能伴有近視度數加深,單眼復視(單眼看東西時出現多個物像)等癥狀。一般不伴有眼紅眼痛。目前雖然有許多藥物,但尚無藥物可以使白內障的進程逆轉。所以真正可以使患者視力恢復的治療仍是手術治療。 手術的目的是為了去除已經混濁的晶狀體,並植入人工晶狀體以提高患者的視力。以前由於手術技術的限制,皮質型白內障的手術需要到成熟期才可以進行,此時患者基本上已經沒有視力。目前白內障手術的技術已經突破此限制,其適應症大大放寬。 分類及成因 由於水晶體的化學成分改變而導致混濁,其中以老化所造成的老年性白內障最為常見。依不同類型的白內障造成原因如下: 1.老年性白內障:由於長期紫外線的傷害及組織的老化,導致水晶體變硬而混濁所致,所謂人老「珠」黃,指的就是這一型的白內障,最早在四十歲左右即可發生。 2.先天性白內障:可能因為遺傳或者是胎兒時期的感染,在出生時即已發生水晶體混濁。 3.外傷性白內障:眼睛受傷也可造成白內障,舉凡撞擊、穿刺傷、電擊、高熱、化學藥品灼傷等,皆可能傷及水晶體。 4.續發性白內障:可續發於眼疾或全身性疾病,如青光眼、虹彩炎、糖尿病等,或是受某些特定的感染、藥物誘導,如皮質類固醇。 症狀主要症狀為無痛無癢的進行性視力減退,會覺得有一層毛玻璃擋在眼前。其他症狀包括,複視、畏光、眩光、色彩失去鮮明度,和經常需要更換眼鏡等症狀。水晶體也可能吸收水分而增厚,導致近視者度數加深,而老花眼者閱讀書報反而不需戴眼鏡,以為得到眼睛的「第二春」。當視力再也無法以更換眼鏡度數來改善時,就到了必須積極治療的時候。 預防 有關預防白內障的方法,目前科學上還沒有定論。但有醫學文獻表明,佩戴防紫外線光的墨鏡有可能減慢白內障的發展。 如何治療 手術摘除是唯一有效的治療。當白內障嚴重到影響個人的工作及日常生活,便是考慮接受白內障手術的時候了,不論視力是多少。 |
|
|
白內障 手術分類
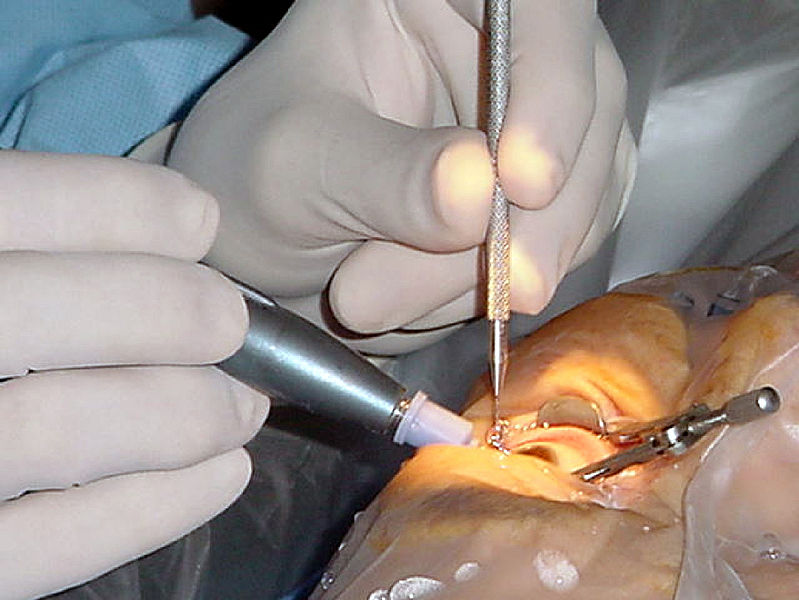
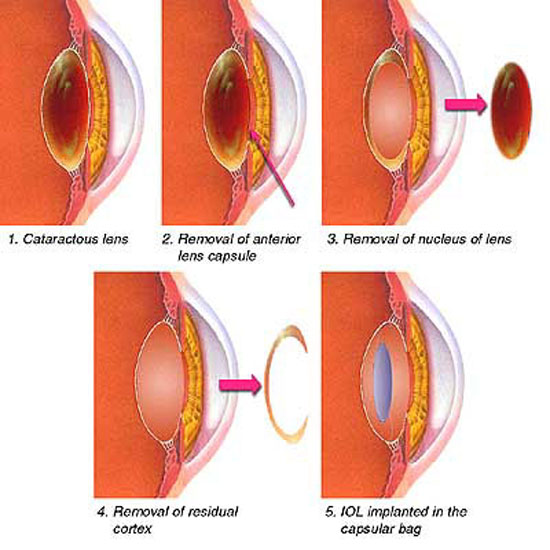
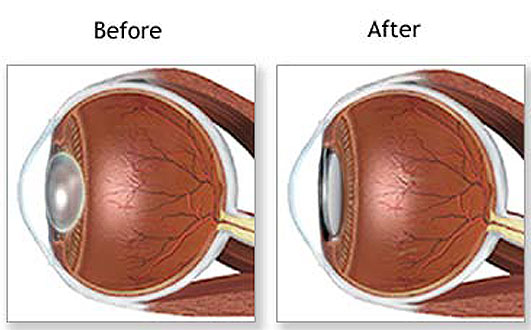
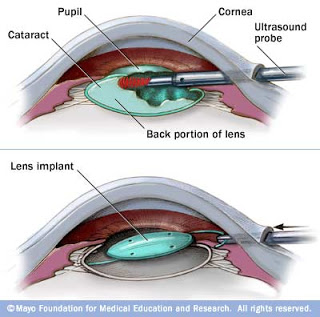
天然的晶體具有一個囊袋,即晶狀體囊,按照手術摘除時晶體核於囊袋的關係,分為囊內摘除和囊外摘除。在摘除混濁的晶體後,往往還要放入一個人工晶體,人工晶體的位置可以放置在前房或者後房,在後房又可以在囊內或者囊外。放置人工晶體除了可以恢復視力,還可以恢複眼內的解剖關係,防止前部玻璃體的脫出,如果前部玻璃體從玻璃體腔內脫出到前房和角膜或者虹膜組織相粘連,可能會對視網膜造成牽拉。 白內障囊內摘出術(Intracapsular cataract extraction, ICCE):大切口切開角鞏膜緣,進入後用冷凍頭凍住晶體,向外牽拉造成懸韌帶的斷裂,娩出晶體。 白內障囊外摘除術(Extracapsular cataract extraction, ECCE):開關式截囊,娩出晶體核,同步灌注抽吸清除殘餘晶狀體皮質。 超聲乳化晶體摘除術(Phacoemulsification, Phaco):連續環形撕囊,超聲乳化晶體核,同步灌注抽吸清除晶狀體皮質。 在後兩種手術完成後,通常植入人工晶體以獲得理想的裸眼視力。 手術適應症 早期的手術方式,例如ICCE需要等待晶體完全混濁以後才能施行,即等待晶體「成熟」。但是對於現在常用的phaco而言,成熟期的白內障反而不好做,因此早已不把白內障是否成熟作為手術適應症的指標了。由於醫學知識普及的不足,還有很多人認為需要等待白內障成熟以後才能做手術。至於白內障何時手術合適,很大程度上取決於病人自身的願望,可以把白內障是否影響日常生活作為一個指標, 手術禁忌症 空腹血糖>=8.0mmol/L 過高的血壓 不能平臥 角膜內皮細胞數量過少 手術過程 以超聲乳化晶體摘除術+人工晶體植入術為例: 球後麻醉,注射2%利多卡因2.5mL。 常規消毒鋪巾。 沿角膜緣,從11點至12點切開角膜。 角膜緣外2mm,從11點至12點垂直板層切開鞏膜的1/3-1/2,用隧道刀水平分離,進入透明的角膜,形成隧道切口,以穿刺刀在11:30穿入前房,注入粘彈劑。 在2點處穿刺前房,並刺入晶體前囊。 連續環形撕囊。 水分離、水分層。 超聲乳化晶體摘除。 吸取皮質,拋光前囊。 植入人工晶體。 灌注抽吸,去除殘餘皮質及粘彈劑。 封閉結膜傷口。 結膜下注射激素與抗生素。 術後常規應用糖皮質激素及非甾體抗炎眼藥水。 術後應當注意事項 一、開刀後若需點滴眼藥水,請注意 (1)請先用肥皂及清水洗手、擦乾。 (2)病人的姿勢最好是躺著(坐著也可以)。 (3)頭稍微往後仰,用食指拉下下眼瞼。 (4)眼睛往上看,另一支手點下藥水或藥膏。 (5)放開下眼瞼,輕輕閉上眼睛,休息三分鐘。 二、為保護眼睛,外出或睡覺時,請戴上眼罩。 三、行動宜緩慢,最好有人陪伴。 四、如覺得有下列情形,請速回院檢查: (1)眼睛刺痛、發紅。 (2)眼睛分泌物很多。 (3)不斷流眼淚。 (4)視力突然減退。 五、未經醫師許可前,請盡量避免下列動作,以免眼壓增高,影響傷口: (1)請勿抱小孩或提重物等粗重工作。 (2)請勿彎腰撿東西或自己洗頭。 (3)請勿用手或手帕用力揉眼睛。 (4)請勿朝向眼睛開刀那一側睡覺。 (5)勿吃硬的東西,如瓜子、蠶豆。 (6)勿吃刺激性的東西,如辣椒、煙。 (7)如有便秘,不可用力。 (8)避免咳嗽。 Click here to edit.
|
|
白內障 問答
白內障是如何形成的?它一定是老化的結果嗎? •白內障發生的原困迄無確切的根據,只知是由於水晶體的化學成分改變而導致混濁。 •老化是最常見的原因。除了老化以外,其他原因,有:眼睛受傷、眼睛或身體的疾病、遺傳或先天異常等。 •老年性白內障為最常見的一種,乃水晶體老化而變硬混濁所致,常發生於老年人,所謂人老"珠"黃。珠,指的就是水晶體。此型白內障不一定發生於年紀很大的人,最早在四十歲左右即可發生。 •嬰兒也可能因遺傳因素而發生白內障。其中在懷孕期間由於感染或發炎所造成的,我們稱之為 "先天性白內障"-意即在出生時即已出現。 •眼睛受傷也會造成白內障,舉凡硬物撞擊、穿刺傷、切傷、高熱、電擊、化學物灼傷,皆可傷及水晶體,導致"外傷性白內障"。 •另外,某些特定的感染、藥物(如皮質類固醇"俗稱美國仙丹)、眼疾、糖尿病等,亦會造成所謂的"併發性白內障"。 白內障除了視力模糊外,會痛會癢嗎? •白內障主要的症狀為無痛、無癢的進行性視力減退。依白內障的位置和程度的不同,病患可能視力減退,也可能毫無所覺。 •一般而言,白內障位於水晶體邊緣者較無症狀,位於中央偏後者,症狀較為嚴重。可能有視力模糊、複視、畏光、眩光、色彩失去鮮明度、和需經常更換眼鏡等症狀。 •水晶體也可能吸收水分而增厚。因此,近視者其眼鏡度數會加深;"老花眼"者閱讀書報,反而不需戴眼鏡。這種現象,稱之為"第二春之視力"。當白內障嚴重到一定程度,視力再也無法以更換眼鏡度數來改善,此時瞳孔看起來不再是黑色,而呈白色或淡黃色。 白內障由眼外觀察就能診斷嗎? 一般而言,白內障無法由眼外直接觀察診斷。眼科醫師診斷白內障時,會借助儀器的輔助來確定水晶體混濁的形狀、大小及位置。 白內障如何治療?點眼藥有效嗎? •目前為止,尚無藥物可以治療白內障。點眼藥,充其量只能減緩它的進行速度而已。 •手術摘除是唯一有效的治療。當白內障嚴重到影響個人的工作及日常生活品質時,便是考慮摘除白內障的時機了,不論視力是多少,也不管它是否"熟"了。 白內障手術是怎麼一回事? •白內障摘除手術是在全身或局部麻醉下施行,將混濁的水晶體在顯微手術下摘除乾淨。 •一旦水晶體被摘除,其屈光功能必須由人工的鏡片來代替。病患可於手術後配戴高度遠視鏡片 (凸透鏡)、隱形跟鏡、或置放"眼內人工水晶體",來改善視力。但人工水晶體己成為目前最被普遍接受的選擇。 白內障手術成功率如何? •儘管有先進的技術和人工水晶體的幫忙,手術後的視力仍決定於眼球本身的健康與否,特別是視網膜和視神經的狀況。 •儘管白內障手術有很高的成功率(將近百分之九十五),手術的併發症仍是不可避免的,沒有人能保證手術絕對成功。 白內障不治療會不會瞎掉? 白內障程度嚴重者,視力會很差,甚至無法應付日常生活,形成"法律上的盲"。白內障可能引起"續發性青光眼"或"虹彩炎"等併發症,若治療不當,則終至眼盲也有可能。 白內障可以用"雷射"來治療嗎? 白內障不能用"雷射"來治療。白內障手術後的一段時間,因為後囊再度增厚而混濁的情形,稱為"後發白內障"。這時,可以借助雷射將混濁的後囊打開。雷射治療白內障,指的是這種"後發白內障"的情形。 聽說白內障可以用超音波來治療,是怎麼回事? 所謂"超音波晶體乳化術"是使用超音波將白內障的晶體核乳糜化,再將其吸乾淨的一種手術方法。它的好處是切口很小、手術後傷口復原很快、散光的機率較低。但手術儀器昂貴、技術較難、且手術併發症也不少。此項手術的目的與一般白內障手術相同,也是施行"囊外晶體摘除",以便置放"後房人工水晶體"。 白內障可以預防嗎? 目前為止,尚無藥物-眼藥、注射劑、或其他方法來預防白內障。市面上雖然有販賣白內障眼藥水或內服藥片及特殊食品的販賣,充其量只能略為延緩白內障之進行。 |
|
Cataract
A cataract is a clouding of the lens inside the eye which leads to a decrease in vision. It is the most common cause of blindness and is conventionally treated with surgery. Visual loss occurs because opacification of the lens obstructs light from passing and being focused on to the retina at the back of the eye. It is most commonly due to biological aging but there are a wide variety of other causes. Over time, yellow-brown pigment is deposited within the lens and this, together with disruption of the normal architecture of the lens fibers, leads to reduced transmission of light, which in turn leads to visual problems. Those with cataracts commonly experience difficulty in appreciating colors and changes in contrast, driving, reading, recognizing faces, and coping with glare from bright lights. Signs and Symptoms Bilateral cataracts in an infant due to congenital rubella syndrome Signs and symptoms vary depending on the type of cataract, though there is considerable overlap. People with nuclear sclerotic or brunescent cataracts often notice a reduction of vision. Those with posterior supcapsular cataracts usually complain of glare as their major symptom. The severity of cataract formation, assuming that no other eye disease is present, is judged primarily by visual acuity test. The appropriateness of surgery depends on a patient's particular functional and visual needs and other risk factors, all of which may vary widely. Causes Age Age is the most common cause. Lens proteins denature and degrade over time and this process is accelerated by diseases such as diabetes and hypertension. With the passage of time, environmental factors including toxins, radiation and UV light have an accumulative effect. These effects are worsened by the loss of protective and restorative mechanisms due to alterations in gene expression and chemical processes within the eye. Treatment Surgical Cataract surgery Slit lamp photo of posterior capsular opacification visible a few months after implantation of intraocular lens in eye, seen on retroillumination Cataract removal can be performed at any stage and no longer requires ripening of the lens. Surgery is usually 'outpatient' and performed using local anesthesia. Approximately 90% of patients can achieve a corrected vision of 20/40 or better after surgery. Several recent evaluations found that surgery can only meet expectations when there is significant functional impairment from poor vision prior to surgery. Visual function estimates such as VF-14 have been found to give more realistic estimates than visual acuity testing alone. In some developed countries a trend to overuse cataract surgery has been noted which may lead to disappointing results. Extracapsular cataract extraction (ECCE), consists of removing the lens manually, but leaving the majority of the capsule intact. The lens is expressed through a 10–12 mm incision which is closed with sutures at the end of surgery. Extracapsular extraction is less frequently performed than phacoemulsification but can be useful when dealing with very hard cataracts or other situations where emulsification is problematic. Manual small incision cataract surgery (MSICS) has evolved from extracapsular cataract extraction. In MSICS, the lens is removed through a self-sealing scleral tunnel wound in the sclera which, ideally, is watertight and does not require suturing. Although "small", the incision is still markedly larger than the portal in phacoemulsion. This surgery is increasingly popular in the developing world where access to phacoemulsification is still limited. Intracapsular cataract extraction (ICCE) is rarely performed. The lens and surrounding capsule are removed in one piece through a large incision while pressure is applied to the vitreous membrane. The surgery has a high rate of complications. Phacoemulsification is one of the most widely used cataract surgery nowadays. This procedure is using ultrasonic energy (U/S) to emulsifying the cataract lens. One technique in phacoemulsification is Micro Incision cataract Surgery (MICS) that is performed by a less than 2 mm (sub 2) micro incision and followed by wound assisted insertion of MICS intraocular lens (IOL). The newest procedure in cataract surgery is called Femtosecond Laser Cataract Surgery (FLCS) that is using femtosecond laser to perform capsulorhexxis, lens softening, clear corneal incision and limbal relaxing incision. This procedure still uses phaco machine to perform aspiration of lens material and perform the maneuver of irrigation-aspiration. Phacoemulsification, typically comprises five steps, not including the anaesthetic. Anaesthetic - The eye is numbed with either a subtenon injection around the eye or using simple eye drops. Corneal Incision - Two cuts are made through the clear cornea to allow insertion of instruments into the eye. Capsulorhexis - A needle or small pair of forceps is used to create a circular hole in the capsule (or bag) in which the lens sits. Phacoemulsification - A handheld probe is used to break up and emulsify the lens into liquid using the energy of ultrasound waves. The resulting 'emulsion' is sucked away. Irrigation and Aspiration - The cortex which is the soft outer layer of the cataract is aspirated or sucked away. Fluid removed is continually replaced with a salt solution to prevent collapse of the structure of the anterior chamber (the front part of the eye). Lens insertion - A plastic foldable lens is inserted to the capsular bag that is used to contain the natural lens. Some surgeons will also inject an antibiotic in to the eye to reduce the risk of infection. The final step is to inject salt water in to the corneal wounds to cause the area to swell and seal the incision. Post-operative care The post-operative recovery period (the period after cataract extraction is done) is usually short. The patient is usually ambulatory on the day of surgery but is advised to move cautiously and avoid straining or heavy lifting for about a month. The eye is usually patched on the day of surgery and at night using an eye shield is often suggested for several days after surgery. In all types of surgery, the cataractous lens is removed and replaced with an artificial lens, known as intraocular lens, which stays in the eye permanently. Intraocular lenses are usually monofocal, correcting for either distance or near vision, however, multifocal lenses may be implanted to improve near and distance vision simultaneously, but these lenses may increase the chance of unsatisfactory vision. Complications Serious complications of cataract surgery are retinal detachment and endophthalmitis. In both cases, patients will notice a sudden decrease in vision. In endophthalmitis, patients will often describe pain. Retinal detachment frequently presents with unilateral visual field defects, blurring of vision, flashes of light or floating spots. The risk of retinal detachment was estimated as approximately 0.4% within 5.5 years, corresponding to a 2.3x risk increase compared to naturally expected incidence, older studies reporting a substantially higher risk. The incidence is increasing over time in approximately linear manner and the risk increase lasts for at least 20 years after the procedure. Particular risk factors are younger age, male sex, longer axial length and complications during surgery. In highest risk group of patients the incidence of pseudophakic retinal detachment may be as high as 20%. The risk of endophthalmitis occurring after surgery is less than 1 in 1000. Corneal oedema and cystoid macular oedema are less serious but more common and occur because of persistent swelling at the front of the eye in corneal oedema or back of the eye in cystoid macular oedema. They are normally the result of excessive inflammation following surgery and in both cases, patients may notice blurred, foggy vision. They normally improve with time and with application of anti-inflammatory drops. The risk of either occurring is around 1 in 100. Posterior capsular opacification, also known as after cataract, is a condition in which months or years after successful cataract surgery, vision deteriorates or problems with glare and light scattering recur. This is usually due to thickening of the back or posterior capsule surrounding the implanted lens, so-called ' posterior lens capsule opacification'. Growth of natural lens cells remaining after the natural lens was removed may be the cause, and the younger the patient, the greater the chance of this occurring. Management involves cutting a small, circular area in the posterior capsule with targeted beams of energy from a laser, a procedure called YAG laser capsulotomy, after the type of laser used. The laser can be aimed very accurately and the small part of the capsule which is cut falls harmlessly to the bottom of the inside of the eye. This procedure leaves sufficient capsule to hold the lens in place but removes enough to allow light to pass directly through to the retina. Serious side effects are rare.[34] Posterior capsular opacification is common and occurs following up to 1 in 4 operations but these rates are decreasing following the introduction of modern intraocular lenses together with a better understanding of the causes. Epidemiology Disability-adjusted life year for cataracts per 100,000 inhabitants in 2004. Age-related cataracts are responsible for 51% of world blindness, about 20 million people. Globally, cataracts cause moderate to severe disability in 53.8 million (2004), 52.2 million of whom are in low and middle income countries. In many countries surgical services are inadequate, and cataracts remain the leading cause of blindness. Even where surgical services are available, low vision associated with cataracts may still be prevalent as a result of long waits for, and barriers to, surgery - such as cost, lack of information and transportation problems. In the United States, age-related lens changes have been reported in 42% between the ages of 52 and 64, 60% between the ages 65 and 74, and 91% between the ages of 75 and 85. Cataracts affect nearly 22 million Americans age 40 and older. By age 80, more than half of all Americans have cataracts. Direct medical costs for cataract treatment are estimated at $6.8 billion annually. In the Eastern Mediterranean Region, Cataracts are responsible for over 51% of blindness. Access to eye care in many countries on this region is limited. |