現在位置 : 病症 > 胃腸病 > 胰臟炎與胰臟疾病 - Pancreatitis
|
認識你的胰臟
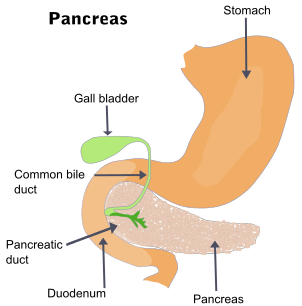
全民健康基金會 外分泌腺:有導管可將分泌物經由導管排到體內,例如:口腔中的唾液腺及眼睛周圍的淚腺等。 內分泌腺:沒有導管,分泌液直接滲透到腺體旁邊的微血管中進入血液,分泌量少但功能卻很大,例如:甲狀腺、睪丸及腎上腺等。 胰臟對很多人來說可能很熟悉,因為非常耳熟的糖尿病就是胰臟出了問題,而胰臟的癌症---胰臟癌,非常的惡性,也令人心驚膽戰。但是胰臟這個器官到底長在那裡?有什麼真正的功能?可能許多人一知半解。 胰臟長在那裡? 胰臟長的扁扁長長的,橫躺在上腹部的中央,有頭、頸、體與尾4個部位,躲在腹膜後,在肝臟和胃的後面,橫臥於第1及第2腰椎的前方,彷彿是螢光幕後的工作人員,默默工作,鮮少有機會看到它出來亮相,另外它的塊頭也不大,成人的胰臟長約12至15公分,厚1至3公分,重約60至125公克。 胰臟有什麼功能? 整個胰臟由外分泌腺細胞所組成,其中點綴著內分泌腺細胞的小群集,叫做胰島腺。因此它具有消化外來食物的外分泌功能;也具有調節體內血糖高低的內分泌功能,是人體中具有外分泌與內分泌的器官。 胰臟每天約分泌1000至1200西西的消化液,內含多種消化酶,如:消化碳水化合物的澱粉酶 (amylase),消化蛋白質的胰蛋白酶(trypsin)和胰凝乳蛋白酶 (chymotrypsin),消化脂質的脂肪酶(lipase)等,幫助食物消化成更細小的分子,以利人體吸收。 全世界每10秒鐘就有1人因糖尿病而死亡,有2人被診斷為糖尿病,而掌控糖尿病有關的醣類代謝激素─胰島素(Insulin),就是由胰臟中胰島腺的β細胞所分泌,因此胰臟扮演著人體中重要的內分泌腺體,經由分泌的內分泌激素(胰島素及昇糖素 glucagon等),調節葡萄糖等碳水化合物的代謝,健全的胰臟功能讓我們免當「糖尿」人。 胰臟出問題會有什麼後果? 外分泌部分出現問題 當胰臟功能受損(例如:慢性胰臟炎引起胰臟纖維化或胰臟手術切除等),消化食物的外分泌功能會先受到波及,若外分泌功能缺損至某一程度時,則會嚴重影響人體消化的機能,容易產生下痢、解脂肪便,甚至引起體重減輕的現象。 因此經常與好友喝酒大快朵頤,或有膽結石、高三酸甘油脂、高血鈣與家族有胰臟炎病史等人,要特別注意這個躲在幕後器官,有可能會發生急性胰臟發炎等現象,包括突然而持續的上腹部劇烈疼痛、或合併噁心和嘔吐等症狀,這種疼痛感會因走路或躺平而加重,坐起向前彎時疼痛才會稍為緩和,有時候疼痛更會放射到背部,嚴重的話會合併發燒、心跳加速,甚至產生休克危及生命。 因此懷疑有急性胰臟炎的時候,要立即就醫,檢驗血清中澱粉酶及脂肪酶是否升高,有時需安排腹部影像檢查如超音波或電腦斷層,以評估胰臟發炎的嚴重程度,必要時還需住院注射足夠的點滴輸液與電解質,保持空腹使胰臟休息,嚴重者若合併器官衰竭(如呼衰竭吸、急性腎衰竭等),有時甚至須要轉至加護病房觀察與治療。 內分泌部分出現問題 胰臟製造的胰島素,它可幫助吃進去的澱粉類食物轉變成葡萄糖,提供身體熱能,但若是胰臟內分泌功能有缺陷或失調,不能產生足夠的胰島素或身體產生胰島素的阻抗性,讓葡萄糖無法進入細胞,血糖濃度升高就會引起人人耳熟能詳的糖尿病。未良好控制的糖尿病則會造成視網膜病變、腎臟病變、神經病變與心血管疾病,而導致失明、洗腎、截肢、中風等嚴重的併發症。 另外有少數人罹患胰島腺瘤,反而會使得胰細胞異常分泌胰島素,因過量的胰島素而造成低血糖的症狀,如:飢餓、冒冷汗及發抖等,嚴重時還會危及生命。 糖尿病的高危險群 1. 家族有糖尿病史患者 2. 肥胖及缺乏運動者 3. 年紀大於45歲 4. 懷孕婦女 5. 服用特殊藥物,如:乙型阻斷劑、類固醇,蛋白分解酵素抑制劑等 胰臟癌常未能早期發現 胰臟細胞惡化產生病變,由於胰臟位置的特性,產生腫瘤時不容易被發現,發現時胰臟癌通常都很末期,存活期很短。 腫癌若長在胰臟頭部位置,由於容易造成阻塞膽汁流通,出現黃疸,較易被發現,此時若及早發現可能可以手術切除,但若長在胰臟尾部,通常要到腹水與體重減輕等症狀出現就醫才發現,而此時的胰臟癌大多已是晚期,預後不佳,因此胰臟癌的高危險群民眾,若有上腹痛等症狀產生,應盡快做進一步包括腹部影像及抽血檢查,以期能早期發現早期治療。 胰臟癌的高危險群 1. 年紀60歲以上男性 2. 有抽菸習慣的人 3. 有糖尿病史或家族有糖尿病史者 4. 慢性胰臟炎患者 5 家族有胰臟癌病史患者 6. 曾做部分胃切除手術者 如何保護胰臟健康? 去除會引發胰臟發炎的危險因子就是最好的保護之道,因此避免抽菸、長期喝酒且飲食清淡低油脂,將可降低胰臟炎的發生;另外胰臟癌的高危險群民眾,更應定期追蹤檢查;而糖尿病高危險群的人,也應定期做空腹血糖篩檢,以早期發現早期治療。 |
|
胰臟炎
胰臟的功能是幫助消化,它會分泌胰液,胰液中含有澱粉酶、脂肪酶、及蛋白酶泌等不具活性的外分泌消化酵素,當人體吃下食物時,這些酵素可幫助消化分解食物中的脂肪、蛋白質以及醣類。胰臟同時釋放內分泌荷爾蒙,包含胰島素及升醣素至血液中,以維持血糖的恆定。正常情況下,胰臟所分泌不具活性的消化酵素要在腸道才會被活化,當這些具活性的酵素在胰臟時即會消化胰臟本身,而導致胰臟炎。 胰臟炎(胰腺炎)是發炎的胰腺導致,需要立即就醫。它會產生胰腺酶(尤其是胰蛋白酶)的異常。這可能是急性即突然開始並持續數天,或慢性即多年來發生幾次。這有多方面的原因。 急性胰腺炎最常見的症狀是嚴重的上腹部燒灼樣疼痛放射到背部。疼痛會有所不同,這取決於嚴重程度和內部出血。血壓升高或減少,心臟出血率和呼吸率也會升高。慢性胰腺炎可導致糖尿病或胰臟癌。不明原因的體重減輕,可能會出現胰腺酶的缺乏阻礙了消化。 原因 80%的胰腺炎是由於攝入酒精過多和膽結石,膽結石是一種最常見的急性胰腺炎的病因。酒精是一種最常見的慢性胰腺炎的病因。 其他常見的原因包括外傷、腮腺炎、自身免疫性疾病、蠍子蜇傷、高血鈣、血中甘油三酯高、低溫。胰腺分裂的胰腺,可依據一些經常性的情況下,是一種常見的先天性畸形。懷孕可以是一個原因,可能是因為懷孕導致血中甘油三酯升高。 不太常見的原因包括胰腺癌和胰管結石。 慢性胰臟炎 慢性胰臟炎的症狀 : (1).大多數患者出現腹痛現象 (2).當進食或喝酒時疼痛的症狀加重 (3). 患者有噁心、嘔吐、體重減輕、脂肪便等 當胰臟持續受損,可能會演變成慢性胰臟炎,造成消化酵素攻擊破壞胰臟和周遭的組織,導致慢性胰臟炎的主要原因有長期酗酒、胰管阻塞、胰臟外傷、遺傳因素、自發性因素。慢性胰臟炎好發於中年人口,男性多於女性,而其他相關因素尚有高血脂症、高鈣血症、藥物因素、囊性纖維化、自體免疫疾病等。大多數的慢性胰臟炎患者會出現腹痛的症狀,當進食或喝酒時使疼痛的症狀惡化,但有部分患者因為胰臟炎惡化,腹痛情形卻消失,這可能是因為胰臟已無法製造消化酵素。其他症狀包含噁心、嘔吐、體重減輕、脂肪便等,這是因為身體無法製造足夠的消化酵素分解食物,營養無法正常吸收,消化功能不佳導致脂肪、蛋白質、醣類排泄至糞便;當胰臟受損無法分泌胰島素時亦可能引發糖尿病。慢性胰臟炎,也隨之增加以下疾病產生的風險:1.膽道阻塞 2.胰臟癌 3.胃出血 4.偽囊腫。 診斷 慢性胰臟炎的診斷一般需考量:臨床症狀、病史、影像學檢查(電腦斷層掃描、內視鏡膽胰管攝影術)、抽血檢驗、尿液及糞便檢查。 治療 解除疼痛為慢性胰臟炎治療的第一步,第二步為調整飲食型態採高碳水化合物及低脂肪飲食。解除疼痛方面,慢性胰臟炎一般先採取內科治療,止痛劑加上抗憂鬱劑以及非類固醇消炎藥對大部分病人有效,當疼痛較嚴重時可能需要止痛貼片,或是住院禁食減少胰臟分泌以減輕疼痛,當慢性胰臟炎的疼痛無法用上述方法減輕時可以考慮外科治療:腹腔神經阻斷術阻斷痛覺傳遞;胰管開口切開或放置胰管支架,以疏通阻塞之胰管;體外震波碎石術排除阻塞胰管的結石,手術將胰管打開接至腸子。 調整飲食型態方面,要絕對禁酒、少量多餐,並將脂肪控制在1天20公克以下,有時醫師會給予胰臟酵素解決消化不良及脂肪便的問題,脂肪消化不良會影響脂溶性維生素的吸收,所以要補充維生素D,有部分的人雖然有飲食及藥物的控制,但是體重仍然減輕,可以補充中鏈三酸甘油酯 ,因為中鏈三酸甘油酯是已經被分解的,不需要膽汁及酵素即可被小腸吸收。 单击此处进行编辑.
|
|
Pancreatitis
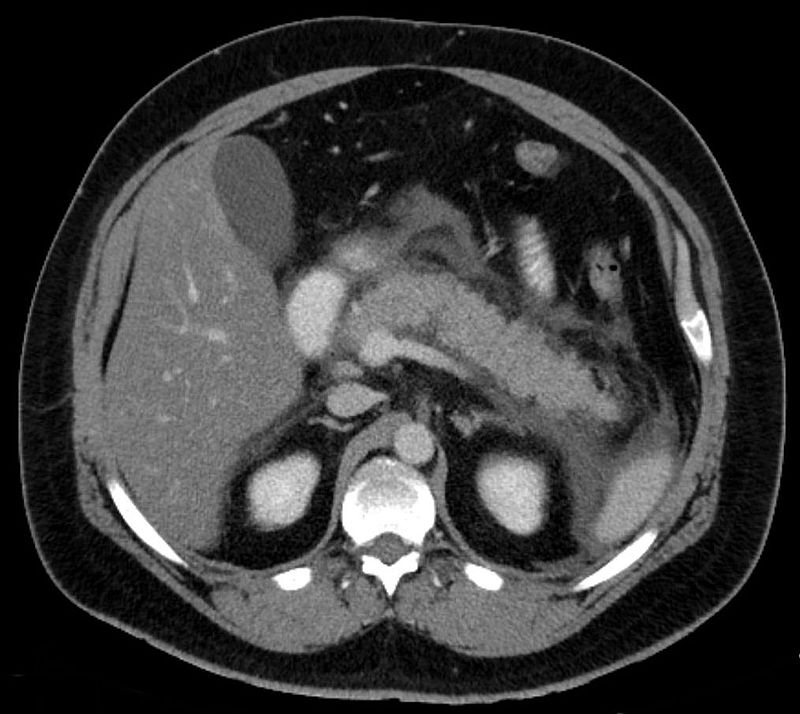
Pancreatitis is inflammation of the pancreas. The pancreas is a large organ behind the stomach which produces digestive enzymes. There are two main types, acute pancreatitis and chronic pancreatitis. Symptoms of pancreatitis include pain in the upper abdomen, nausea and vomiting. The pain often goes into the back and is usually severe. In acute pancreatitis a fever may occur and symptoms typically resolve in a few days. In chronic pancreatitis weight loss, fatty stool, and diarrhea may occur. Complications may include infection, bleeding, diabetes, or problems with other organs. The most common causes of acute pancreatitis are gallstones and heavy alcohol use. Other causes include direct trauma, certain medications, infections such as mumps, and tumors among others. Chronic pancreatitis may develop as a result of acute pancreatitis. It is most commonly due to many years of heavy alcohol use. Other causes include high levels of blood fats, high blood calcium, some medications, and certain genetic disorders such as cystic fibrosis among others. Smoking increases the risk of both acute and chronic pancreatitis. Diagnosis of acute pancreatitis is based on a threefold increase in the blood of either amylase or lipase. In chronic pancreatitis these tests may be normal. Medical imaging such as ultrasound and CT scan may also be useful. Acute pancreatitis is usually treated with intravenous fluids, pain medication, and sometimes antibiotics. Typically no eating or drinking is allowed and a tube may be placed into the stomach. A procedure known as a endoscopic retrograde cholangiopancreatography (ERCP) may be done to open the pancreatic duct if blocked. In those with gallstones the gallbladder is often also removed. In chronic pancreatitis, in addition to the above, temporary feeding through a nasogastric tube may be used to provide adequate nutrition. Long-term dietary changes and pancreatic enzyme replacement may be required. And occasionally surgery is done to remove parts of the pancreas. Acute pancreatitis occurs in about 30 per 100,000 people a year. New cases of chronic pancreatitis develop in about 8 per 100,000 people a year and currently affect about 50 per 100,000 people in the United States. Globally, in 2013 pancreatitis resulted in 123,000 deaths up from 83,000 deaths in 1990. It is more common in men than women. Often chronic pancreatitis starts between the ages of 30 and 40 while it is rare in children. Acute pancreatitis was first described on autopsy in 1882 while chronic pancreatitis was first described in 1946. Signs and symptoms
The most common symptoms of pancreatitis are severe upper abdominal or left upper quadrant burning pain radiating to the back, nausea, and vomiting that is worsened with eating. The physical examination will vary depending on severity and presence of internal bleeding. Blood pressure may be elevated by pain or decreased by dehydration or bleeding. Heart and respiratory rates are often elevated. The abdomen is usually tender but to a lesser degree than the pain itself. As is common in abdominal disease, bowel sounds may be reduced from reflex bowel paralysis. Fever or jaundice may be present. Chronic pancreatitis can lead to diabetes or pancreatic cancer. Unexplained weight loss may occur from a lack of pancreatic enzymes hindering digestion. Causes Eighty percent of cases of pancreatitis are caused by alcohol or gallstones. Gallstones are the single most common cause of acute pancreatitis. Alcohol is the single most common cause of chronic pancreatitis. Some medications are commonly associated with pancreatitis, most commonly corticosteroids such as prednisolone, but also including the HIV drugs didanosine and pentamidine, diuretics, the anticonvulsant valproic acid, the chemotherapeutic agents L-asparaginase and azathioprine, estrogen by way of increased blood triglycerides, and antihyperglycemic agents like metformin, vildagliptin, and sitagliptin. It may be noted here that the drugs which are used to treat conditions which are themselves associated with increased events of pancreatitis may also be incidentally linked to pancreatitis. Examples include statins in dyslipidemia and gliptins in diabetes. According to the Food and Drug Administration's MedWatch Surveillance System and Published Reports Atypical, atypical antipsychotics such as clozapine, risperidone, and olanzapine can also be responsible for causing pancreatitis. Other common causes include trauma, mumps, autoimmune disease, high blood calcium, hypothermia, and endoscopic retrograde cholangiopancreatography (ERCP). Pancreas divisum is a common congenital malformation of the pancreas that may underlie some recurrent cases. Diabetes mellitus type 2 is associated with a 2.8-fold higher risk. Less common causes include pancreatic cancer, pancreatic duct stones, vasculitis (inflammation of the small blood vessels in the pancreas), coxsackievirus infection, and porphyria—particularly acute intermittent porphyria and erythropoietic protoporphyria. There is an inherited form that results in the activation of trypsinogen within the pancreas, leading to autodigestion. Involved genes may include Trypsin 1, which codes for trypsinogen, SPINK1, which codes for a trypsin inhibitor, or cystic fibrosis transmembrane conductance regulator. The mnemonic GETSMASHED is often used to remember the common causes of Pancreatitis: G - Gall stones E - Ethanol T - Trauma S - Steroids M - Mumps A - Autoimmune Pancreatitis S - Scorpion sting H - Hyperlipidaemia, Hypothermia, Hyperparathyroidism E - Endoscopic retrograde cholangiopancreatography D - Drugs commonly azathioprine, valproic acid Infectious causes A number of infectious agents have been recognized as causes of pancreatitis including: Viruses Coxsackie virus Cytomegalovirus Hepatitis B Herpes simplex virus Mumps Varicella-zoster virus Bacteria Legionella Leptospira Mycoplasma Salmonella Fungi Aspergillus Parasites Ascaris Cryptosporidium Toxoplasma Diagnosis Diagnosing pancreatitis requires two of the following: ● Characteristic abdominal pain ● Blood amylase or lipase will be 4-6 times higher than the normal variations, but this will be dependent on the laboratory that is testing the blood. ● Abdominal ultrasound is generally performed first, which is advantageous for the diagnosis of the causes of the pancreas, for example, detecting gallstones, diagnosing alcoholic fatty liver (combined with history of alcohol consumption). They are both the main causes of pancreatitis. Abdominal ultrasound also shows an inflamed pancreas clearly. It is convenient, simple, non-invasive, and inexpensive. ● Characteristic CT scan A CT should be considered after 48h to identify any necrosis Amylase or lipase is frequently part of the diagnosis; lipase is generally considered a better indicator, but this is disputed. Cholecystitis, perforated peptic ulcer, bowel infarction, and diabetic ketoacidosis can mimic pancreatitis by causing similar abdominal pain and elevated enzymes. The diagnosis can be confirmed by ultrasound and/or CT. Treatment The treatment of pancreatitis is supportive and depends on severity. Morphine generally is suitable for pain control. There is a claim that morphine may constrict the sphincter of Oddi, but this is controversial. There are no clinical studies to suggest that morphine can aggravate or cause pancreatitis or cholecystitis. The treatment that is received for acute pancreatitis will depend on whether the diagnosis is for the mild form of the condition, which causes no complications, or the severe form, which can cause serious complications. Mild acute pancreatitis The treatment of mild acute pancreatitis is successfully carried out by admission to a general hospital ward. Traditionally, people were not allowed to eat until the inflammation resolved but more recent evidence suggests early feeding is safe and improves outcomes. Because pancreatitis can cause lung damage and affect normal lung function, oxygen is occasionally delivered through breathing tubes that are connected via the nose. The tubes can then be removed after a few days once it is clear that the condition is improving. Dehydration may result during an episode of acute pancreatitis, so fluids will be provided intravenously. The pain associated with even mild or moderate cases of acute pancreatitis can be severe, which means that a narcotic pain killer may be required. Severe acute pancreatitis Severe pancreatitis is associated with organ failure, necrosis, infected necrosis, pseudocyst and abscess. If diagnosed with severe acute pancreatitis, people will need to be admitted to a high dependency unit or intensive care unit. It is likely that the levels of fluids inside the body will have dropped significantly as it diverts bodily fluids and nutrients in an attempt to repair the pancreas. The drop in fluid levels can lead to a reduction in the volume of blood within the body, which is known as hypovolemic shock. Hypovolemic shock can be life-threatening as it can very quickly starve the body of the oxygen-rich blood that it needs to survive. To avoid going into hypovolemic shock, fluids will be pumped intravenously. Oxygen will be supplied through tubes attached to the nose and ventilation equipment may be used to assist with breathing. Feeding tubes may be used to provide nutrients, combined with appropriate analgesia. As with mild acute pancreatitis, it will be necessary to treat the underlying cause - gallstones, discontinuing medications, cessation of alcohol, etc. If the cause is gallstones, it is likely that an ERCP procedure or removal of the gallbladder will be recommended. The gallbladder should be removed during the same hospital admission or within two weeks of the pancreatitis so as to limit the risk of recurrent pancreatitis. If the cause of pancreatitis is alcohol, cessation of alcohol consumption and treatment for alcohol dependency may improve the pancreatitis. Even if the underlying cause is not related to alcohol consumption, doctors recommend avoiding it for at least six months as this can cause further damage to the pancreas during the recovery process. Oral intake, especially fats, is generally restricted initially but early enteral feeding within 48 hours has been shown to improve clinical outcomes. Fluids and electrolytes are replaced intravenously. Nutritional support is initiated via tube feeding to surpass the portion of the digestive tract most affected by secreted pancreatic enzymes if there is no improvement in the first 72–96 hours of treatment. Prognosis Severe acute pancreatitis has mortality rates around 2-9%, higher where necrosis of the pancreas has occurred. Several scoring systems are used to predict the severity of an attack of pancreatitis. They each combine demographic and laboratory data to estimate severity or probability of death. Examples include APACHE II, Ranson, BISAP, and Glasgow. The Modified Glasgow criteria suggests that a case be considered severe if at least three of the following are true: ● Age > 55 years ● Blood levels: ● PO2 Oxygen < 60mmHg or 7.9kPa ● White blood cells > 15 ● Calcium < 2 mmol/L ● Urea > 16 mmol/L ● Lactate dehydrogenase (LDH) > 600iu/L ● Aspartate transaminase (AST) > 200iu/L ● Albumin < 32g/L ● Glucose > 10 mmol/L This can be remembered using the mnemonic PANCREAS: ● P02 Oxygen < 60mmHg or 7.9kPa ● Age > 55 ● Neutrophilia White blood cells > 15 ● Calcium < 2 mmol/L ● Renal Urea > 16 mmol/L ● Enzymes Lactate dehydrogenase (LDH) > 600iu/L Aspartate transaminase (AST) > 200iu/L ● Albumin < 32g/L ● Sugar Glucose > 10 mmol/L The BISAP score (Blood urea nitrogen level >25 mg/dL, Impaired mental status, Systemic inflammatory response syndrome, age over 60 years, pleural effusion) has been validated as similar to other prognostic scoring systems. Complications Early complications include shock, infection, systemic inflammatory response syndrome, low blood calcium, high blood glucose, and dehydration. Blood loss, dehydration, and fluid leaking into the abdominal cavity (ascites) can lead to kidney failure. Respiratory complications are often severe. Pleural effusion is usually present. Shallow breathing from pain can lead to lung collapse. Pancreatic enzymes may attack the lungs, causing inflammation. Severe inflammation can lead to intra-abdominal hypertension and abdominal compartment syndrome, further impairing renal and respiratory function and potentially requiring management with an open abdomen to relieve the pressure. Late complications include recurrent pancreatitis and the development of pancreatic pseudocysts—collections of pancreatic secretions that have been walled off by scar tissue. These may cause pain, become infected, rupture and bleed, block the bile duct and cause jaundice, or migrate around the abdomen. Acute necrotizing pancreatitis can lead to a pancreatic abscess, a collection of pus caused by necrosis, liquefaction, and infection. This happens in approximately 3% of cases, or almost 60% of cases involving more than two pseudocysts and gas in the pancreas. |